Diabetes is a chronic medical condition that affects how your body turns food into energy. When you eat, your body breaks down carbohydrates into glucose (sugar), which enters your bloodstream. Insulin, a hormone produced by the pancreas, helps glucose get into your cells to be used as energy. In people with diabetes, the body either doesn’t make enough insulin or can’t use it effectively, leading to high blood sugar levels.
Am I at Risk of Diabetes?
Determining your risk for diabetes involves evaluating several factors, including lifestyle, genetics, and overall health. Here are some key indicators that could suggest a higher risk:
Common Risk Factors
- Family History: If close relatives have diabetes, your risk is higher.
- Age: People over 45 years old have an increased risk.
- Weight: Being overweight or obese can contribute to insulin resistance.
- Sedentary Lifestyle: Lack of physical activity can raise your chances.
- Diet: Consuming excessive sugar or processed foods can impact blood sugar levels.
- High Blood Pressure or Cholesterol: These conditions are often linked to diabetes.
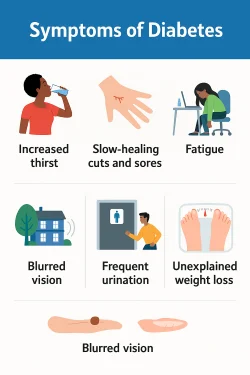
Warning Signs to Watch For
- Frequent urination
- Increased thirst
- Unexplained weight loss
- Constant fatigue
- Blurry vision
- Slow healing of cuts or wounds
Next Steps
If you’re concerned, consider:
- Checking your blood sugar levels through a simple test.
- Consulting a healthcare professional for personalized advice.
- Adopting a healthier lifestyle with balanced nutrition and exercise.
What are the long-term effects of diabetes on health?
The long-term effects of diabetes on health can be serious and widespread, especially if blood sugar levels are not well-managed over time. Here are the major long-term complications:
- Cardiovascular Disease
- Increases risk of heart attacks, strokes, and high blood pressure.
- Diabetes accelerates the development of atherosclerosis (narrowing of arteries).
- Kidney Damage (Diabetic Nephropathy)
- High blood sugar damages the filtering units in kidneys.
- Can lead to chronic kidney disease or kidney failure requiring dialysis or transplant.
- Nerve Damage (Diabetic Neuropathy)
- Leads to pain, tingling, or loss of feeling, especially in feet and hands.
- Can affect digestion, sexual function, and bladder control.
- Eye Damage (Diabetic Retinopathy)
- Damages blood vessels in the retina, potentially leading to blindness.
- Increases risk of glaucoma and cataracts.
- Foot Problems
- Poor circulation and nerve damage can cause slow healing, infections, and ulcers.
- In severe cases, can lead to amputation.
- Skin Conditions
- People with diabetes are more prone to bacterial and fungal infections.
- Dry skin and slow healing can also become persistent issues.
- Hearing Impairment
- Diabetes is linked to higher rates of hearing loss, though the exact cause is still being studied.
- Cognitive Impairment
- Increases risk of Alzheimer’s disease and other forms of dementia, particularly in older adults.
Good news: Many of these complications can be delayed or even prevented by maintaining good blood sugar control, following a healthy lifestyle, and having regular checkups.
How does diabetes impact heart health specifically?
Diabetes has a significant impact on heart health, increasing the risk of various cardiovascular diseases. Here’s how:
- Increased Risk of Heart Disease
- High blood sugar levels can damage blood vessels and the nerves controlling the heart.
- People with diabetes are twice as likely to develop heart disease compared to those without diabetes.
- High Blood Pressure and Cholesterol Issues
- Diabetes often leads to high blood pressure, which forces the heart to work harder.
- Many individuals with diabetes also experience abnormal cholesterol levels, increasing plaque buildup in arteries.
- Atherosclerosis (Hardening of the Arteries)
- Excess glucose in the blood contributes to the narrowing of arteries.
- This condition increases the chances of heart attacks and strokes.
- Increased Risk of Heart Failure
- Damage to blood vessels and high blood pressure can weaken the heart over time.
- The heart may struggle to pump blood efficiently, leading to heart failure.
- Poor Circulation and Blood Clots
- Diabetes can cause blood vessels to become inflamed, reducing circulation.
- Increased risk of clot formation can block blood flow, leading to serious complications like strokes.
How to Protect Your Heart?
- Maintain healthy blood sugar levels through diet and medication.
- Exercise regularly to improve circulation and strengthen the heart.
- Eat heart-friendly foods rich in fiber and healthy fats.
- Manage stress to avoid added strain on the heart.
- Get regular check-ups to monitor heart health and detect issues early.
Diet and Nutrition for Diabetic Health
Maintaining a balanced diet is essential for managing diabetes and overall well-being. Here are key aspects of diabetic-friendly nutrition:
- Understanding Carbohydrates
- Focus on complex carbs like whole grains, vegetables, and legumes.
- Avoid refined sugars and processed foods that cause blood sugar spikes.
- Choosing Healthy Proteins
- Opt for lean proteins such as fish, poultry, tofu, and beans.
- Limit red meat and processed meats, which can increase health risks.
- Incorporating Healthy Fats
- Favor sources like nuts, seeds, olive oil, and avocados.
- Avoid trans fats and excessive saturated fats from fried and processed foods.
- Importance of Fiber
- Helps regulate blood sugar levels and improve digestion.
- Found in fruits, vegetables, whole grains, and nuts.
- Smart Meal Planning
- Balance portions with a mix of protein, healthy fats, and fiber.
- Eat smaller, frequent meals to maintain stable blood sugar levels.
- Hydration and Beverages
- Drink plenty of water to stay hydrated.
- Avoid sugary drinks and excessive caffeine.
- Foods to Limit or Avoid
- Processed foods high in sugar and sodium.
- Alcohol, which can affect blood sugar control.
Is Exercise Really That Important for Diabetes?
Yes, exercise is extremely important for managing diabetes — whether it’s Type 1, Type 2, or prediabetes. Regular physical activity has both immediate and long-term benefits for blood sugar control and overall health.
Why Exercise Matters for Diabetes
- Lowers Blood Sugar Levels
- Exercise helps muscles use glucose (sugar) for energy, reducing the amount in your bloodstream.
- Improves Insulin Sensitivity
- Your body becomes more efficient at using insulin, which helps reduce insulin resistance — a key issue in Type 2 diabetes.
- Aids in Weight Management
- Maintaining a healthy weight improves blood sugar control and can even help reverse prediabetes.
- Boosts Heart Health
- People with diabetes are at higher risk for heart disease — exercise helps lower blood pressure, cholesterol, and strengthens the heart.
- Reduces Stress and Boosts Mood
- Physical activity triggers the release of feel-good hormones, improving mental well-being — which is important for long-term disease management.
- Improves Sleep and Energy Levels
- Better sleep leads to more stable blood sugar levels. Exercise also combats fatigue, a common complaint in people with diabetes.
How Much Exercise Is Recommended?
- 150 minutes per week of moderate-intensity aerobic exercise (e.g., brisk walking, cycling)
- 2–3 days per week of resistance training (e.g., weights, resistance bands)
- Flexibility and balance exercises like yoga or stretching can also help
Tips for Exercising Safely with Diabetes
- Check blood sugar before and after workouts, especially if you take insulin.
- Keep a fast-acting snack (like glucose tablets) nearby to treat low blood sugar.
- Stay hydrated and wear proper footwear to prevent foot injuries.
Bottom Line: Exercise isn’t just important for diabetes — it’s a powerful tool that works like medicine. It’s one of the most effective natural ways to control blood sugar and improve overall quality of life.
Mental and Emotional Well-Being with Diabetes
Living with diabetes is not just a physical journey — it significantly impacts mental and emotional health as well. Managing a chronic condition day after day can feel overwhelming, but recognizing and addressing these emotional challenges is just as important as managing blood sugar.
- Diabetes Burnout
- Constant monitoring, planning, and worry can lead to frustration and exhaustion.
- Common signs include skipping medications, avoiding doctor visits, or feeling hopeless.
- Anxiety and Depression
- People with diabetes are 2 to 3 times more likely to experience depression and anxiety.
- Concerns about long-term health, lifestyle restrictions, or financial stress contribute to this.
- Fear of Hypoglycemia
- Many individuals develop anxiety around low blood sugar episodes, especially at night or in public places.
- Body Image and Self-Esteem
- Weight management, insulin use, or physical symptoms can affect body image and confidence.
Tips for Supporting Mental Health with Diabetes
- Practice Stress-Relief Techniques
- Try meditation, deep breathing, journaling, or yoga.
- Even short walks in nature or mindful moments can ease daily pressure.
- Create a Routine
- Consistent habits in meals, sleep, and medication timing help reduce anxiety and unpredictability.
- Set Small, Achievable Goals
- Progress over perfection. Celebrate small wins like consistent blood sugar checks or walking 15 minutes daily.
- Join a Support Group
- Online or in-person groups can offer encouragement, practical tips, and emotional solidarity.
When to Seek Professional Help
- Persistent sadness, irritability, or feeling emotionally numb
- Thoughts of self-harm or giving up
- Trouble sleeping, eating, or functioning at work or home
A mental health professional can help with coping strategies, therapy, and — when necessary — medication.
Conclusion: Take Control of Diabetes Before It Controls You
Understanding the risks, complications, and management techniques of diabetes is the first step toward a healthier life. From proper nutrition and consistent exercise to mental wellness and routine medical checkups — small, daily actions can lead to big results. Whether you’re at risk or already diagnosed, it’s never too late to take charge of your health and improve your quality of life.
Also Read
References
American Diabetes Association (ADA)
https://www.diabetes.org
Offers comprehensive info on types of diabetes, risk factors, diet, and management tips.
Centers for Disease Control and Prevention (CDC) – Diabetes
https://www.cdc.gov/diabetes
Excellent for statistics, prevention programs, and management resources.
National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)
https://www.niddk.nih.gov/health-information/diabetes
Government-backed medical and research-based diabetes education.
World Health Organization (WHO) – Diabetes
https://www.who.int/health-topics/diabetes
Provides global data, definitions, and action plans for managing diabetes.
Mayo Clinic – Diabetes
https://www.mayoclinic.org/diseases-conditions/diabetes
Offers doctor-reviewed medical information and lifestyle advice.

Add a Comment